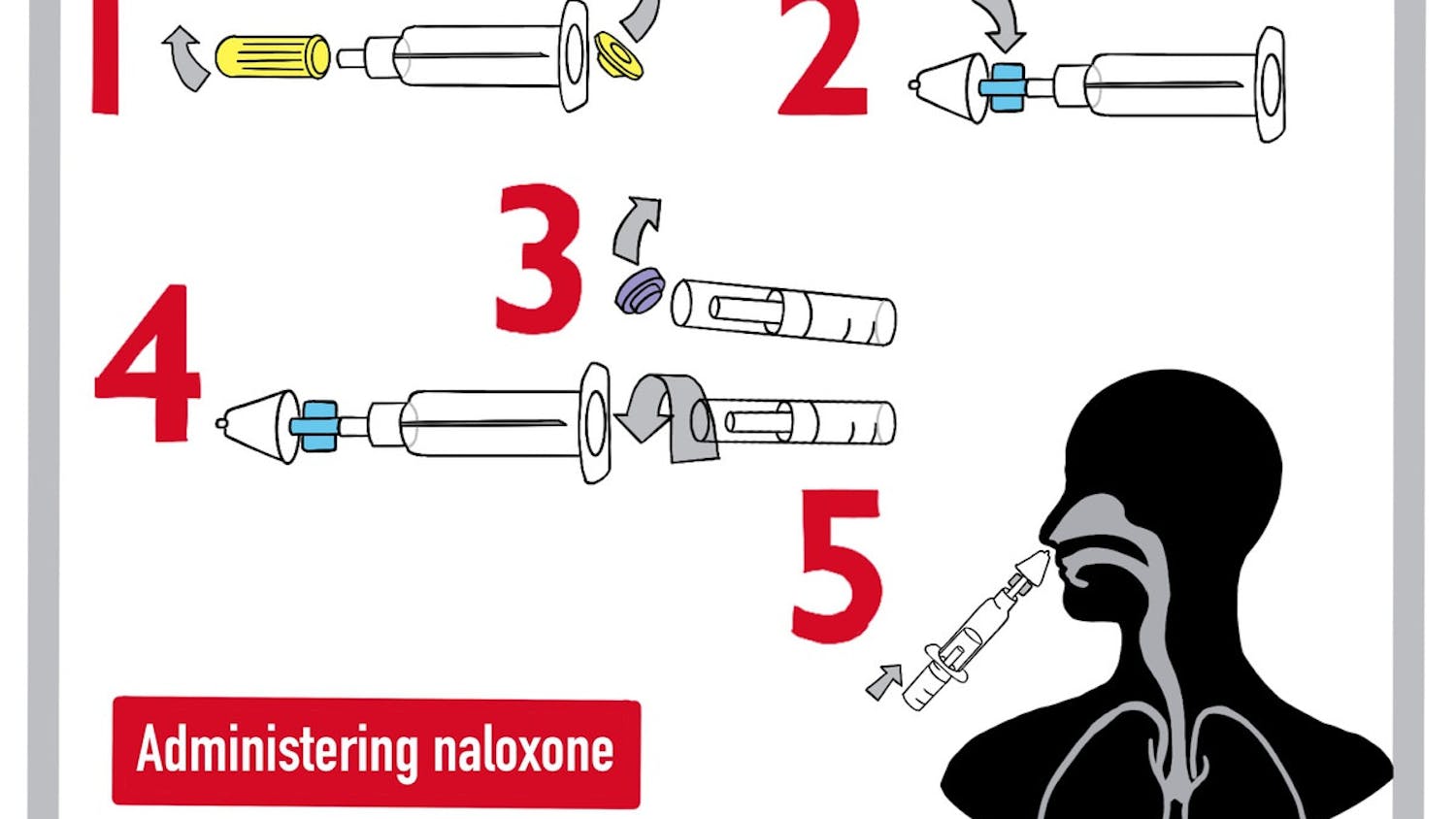
Last month, two federal addiction panels met and unanimously recommended that the Food and Drug Administration approves naloxone — a medicine that reverses the effects of an opioid overdose — for over-the-counter use.
The unanimous push makes it likely that the FDA will approve the recommendation in the near future, the New York Times previously reported. If approved, the decision would impact how pharmacies stock and distribute naloxone.
Opioid overdoses are “the leading cause of accidental death in Rhode Island,” according to the Rhode Island Department of Health. Nationwide, a reported 68,630 people died of an opioid overdose in 2020, and there were 80,411 overdose deaths reported in 2021, according to the National Institute on Drug Abuse.
Individuals in Rhode Island can currently receive naloxone without a prescription from their local pharmacy through a standing order. Rhode Islanders that cannot get the drug through their insurance can also request free naloxone be sent to their house from the state after completing a short training.
Pharmacies like CVS already offer naloxone without individual prescriptions, CVS Retail Communications Manager Ayana Gibbs wrote in an email to The Herald. “We’re committed to expanding access to this life-saving opioid overdose reversal medication and are closely monitoring the FDA’s deliberations to make naloxone available over the counter,” she wrote.
“We should think of over-the-counter naloxone as adding on to the ways in which we make naloxone accessible,” said Brandon Marshall, professor of epidemiology. “It should not mean that we reduce our efforts to distribute naloxone through community-based mechanisms.”
One of the greatest barriers to the current distribution of naloxone is individual stigma from drug use, according to both Marshall and Jeffrey Bratberg, a clinical professor at the University of Rhode Island College of Pharmacy. Bratberg is on a team at the University of Rhode Island that distributes 50,000 kits of naloxone yearly in the state.
Bratberg added that when a prescription is required for naloxone, “your (insurance) provider may find out and ask questions that you don’t want to answer,” making the process uncomfortable for some individuals.
In contrast, when distributed over the counter, the only record is a receipt provided by the store, according to Bratberg.
“By making it over-the-counter, I’m hopeful that we’ll further reduce the stigma and will help people think of naloxone as another type of medication, or another lifesaving tool, like” automated external defibrillators, Marshall said.
The FDA’s recommendation that naloxone be distributed over the counter has both positive and negative implications, according to Bratberg.
“Every overdose that happens is likely because there isn’t naloxone there,” he said. Bratberg noted that while the supply of naloxone isn’t lacking, access to it is limited in certain areas.
“We need to think about how our places and people can have it more easily,” he added. “That’s where I see over-the-counter access being a game changer.”
At the same time, Bratberg explained that insurance companies often stop covering prescriptions that become accessible over the counter. This may create a financial barrier for individuals and stop them from obtaining the life-saving drug, Bratberg said.
For Bratberg, this highlights the importance of maintaining behind-the-counter availability for naloxone, such that “pharmacists can recommend it, clinicians can still prescribe it and it’s insurance-covered.”
Bratberg and Marshall both believe that having multiple channels of access are important — whether through community-based procedures or over-the-counter purchase.
Currently, naloxone is distributed through multiple community channels in Rhode Island. “Let’s say you’re a part of a group at Brown and you want to reduce overdoses. You can apply, we can distribute it to you,” Bratberg said. “You record who it goes to so we know key demographics” of recipients.
“For the people we miss, we can track and ask, ‘Where do we need to augment the system?’” he added.
Bratberg, who has worked on naloxone accessibility and distribution for over a decade, noted that Rhode Island already has a robust network for distributing naloxone.
He added that there are records every time naloxone is dispensed from a pharmacy, so “we have this huge wealth of data to know where it’s going and who needs it.”
“Naloxone should have been over-the-counter 40 years ago,” Bratberg said. “We need to expand our public access so that where there’s a fire extinguisher, where there’s an AED, there’s also naloxone.”
Kelvin Jiang is a section editor for University News and Science & Research at The Herald. Born in Illinois and raised in Palo Alto, CA, Kelvin is concentrating in math-computer science and applied math. He enjoys anything tech-related, being outdoors, and spending time with his cat.