In 2020, 68,630 people in the United States died of an opioid overdose. Opioid overdoses are “the leading cause of accidental death in Rhode Island,” according to the Rhode Island Department of Health, with more than 400 people dying from a drug overdose in 2021. The opioid epidemic continues to affect the Ocean State, especially with the high prevalence of fentanyl, a potent synthetic opioid, commonly added to other drugs.
Naloxone is a medicine that reverses the effects of an opioid overdose. It can be easy to administer and causes immediate opioid withdrawal, experts say.
“Opioid use disorder is a societal thing that we all need to have some claim to or some stake in,” said Geoff Capraro, associate professor of emergency medicine and pediatrics. “If you found a person who's dying of preventable death, you would intervene,” which is why public access to naloxone is so important.
“Every minute really matters,” he added. “Getting naloxone to people really matters.”
An overdose occurs when opioids saturate endogenous opioid receptors, some of which are in the part of the brain which controls breathing. Naloxone, an opioid antagonist, knocks off the opioids binding to the receptors, reducing the opioid’s effect on the body and restoring respiratory function, said Elizabeth Samuels, assistant professor of epidemiology and emergency medicine and consulting assistant medical director for the drug overdose prevention program at the RIDOH.
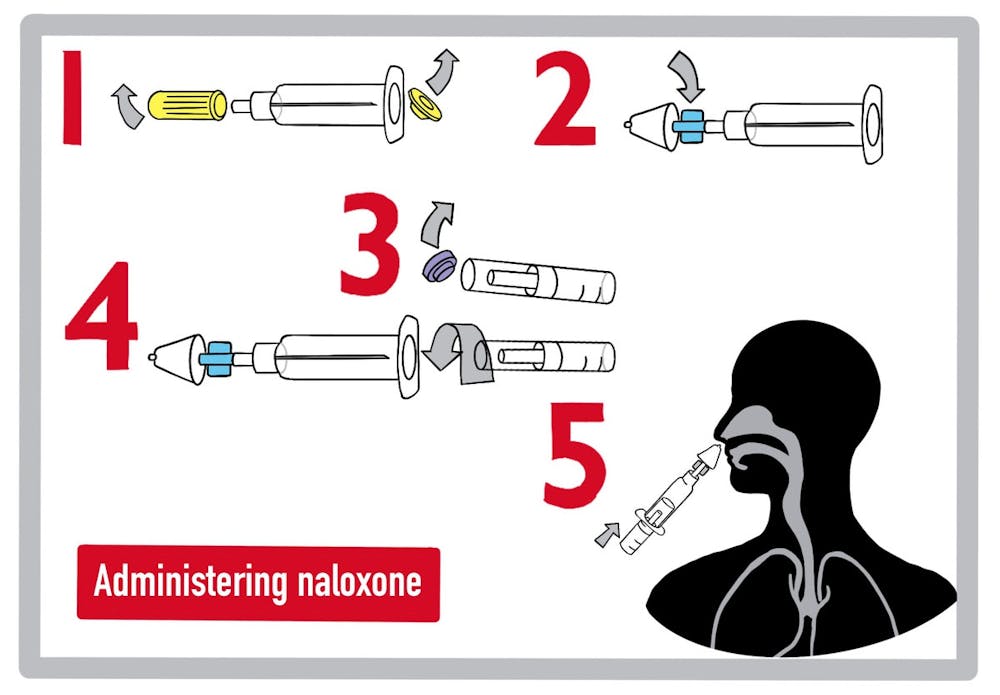
“It’s pretty much a wonder drug,” Capraro said. Naloxone can be administered through an IV, by intramuscular injection or by using a nasal spray, which is the most “user friendly,” he added. Popularly referred to as Narcan, the nasal spray doesn’t require any training for administration and is easily carried in backpacks or pocketbooks.
Failing to administer naloxone fast enough is one of the main factors associated with an overdose death, Samuels said. Since so many overdoses occur in public spaces, public access to naloxone is “extremely important.”
The number of community naloxone kits has risen every year in Rhode Island since 2012. Capraro co-created and implemented the NaloxBox initiative in 2017 to provide public places with “box on a wall” naloxone kits. These kits are similar to automated external defibrillators or fire extinguishers and help make the drug available in high-incidence places, including prisons, soup kitchens, city halls and libraries.
Recently, BWell Health Promotion has partnered with Brown EMS and two local physicians to install boxes around campus containing an AED as well as naloxone “so they’ll be easily accessible to anyone in need,” said Takyah Smith, BWell health promotion specialist and social wellbeing coordinator.
Access to naloxone is increasingly important with the widespread occurrence of fentanyl in stimulants and “party drugs,” Capraro said. Illicit fentanyl was introduced to the opioid drug supply in 2014, according to Samuels, and has been present in 77% of accidental overdose deaths in Rhode Island.
BWell offers trainings for University community members on the use and administration of naloxone every semester — including multiple times this year, Smith said. Participants learn how to recognize the signs of an opioid overdose and how to administer naloxone.
When individuals can ask questions and have an open discussion, “I feel like it definitely decreases the stigma that is currently around opioid use or drug use,” Smith said.
Training participants can also learn about the opioid crisis in the United States and within Rhode Island. During the training, they receive their own dose of naloxone and fentanyl strips, which can detect the presence of fentanyl in various drugs prior to ingestion, according to the Center for Disease Control and Prevention. More information on these trainings can be found on BWell’s website.
Initiatives by RIDOH’s Drug Overdose Prevention Program include efforts to increase naloxone access and distribution, support street outreach and provide harm reduction services, according to Samuels. She is currently working on implementing hospital standards of care for the treatment of overdose and opioid use disorder, she said.
“There's been a lot of really amazing work to expand public health and medical approaches to substance use and addictions,” she added. “But we have much, much further to go.
“I think people who are … supervising a lot of people or responsible for a lot of people definitely need training on how to use and administer naloxone,” Samuels said. “It's something we need to kind of normalize and institutionalize for how we care for each other and the communities that we’re a part of.”
Haley Sandlow is a contributing editor covering science and research. She is a junior from Chicago, Illinois studying English and French.