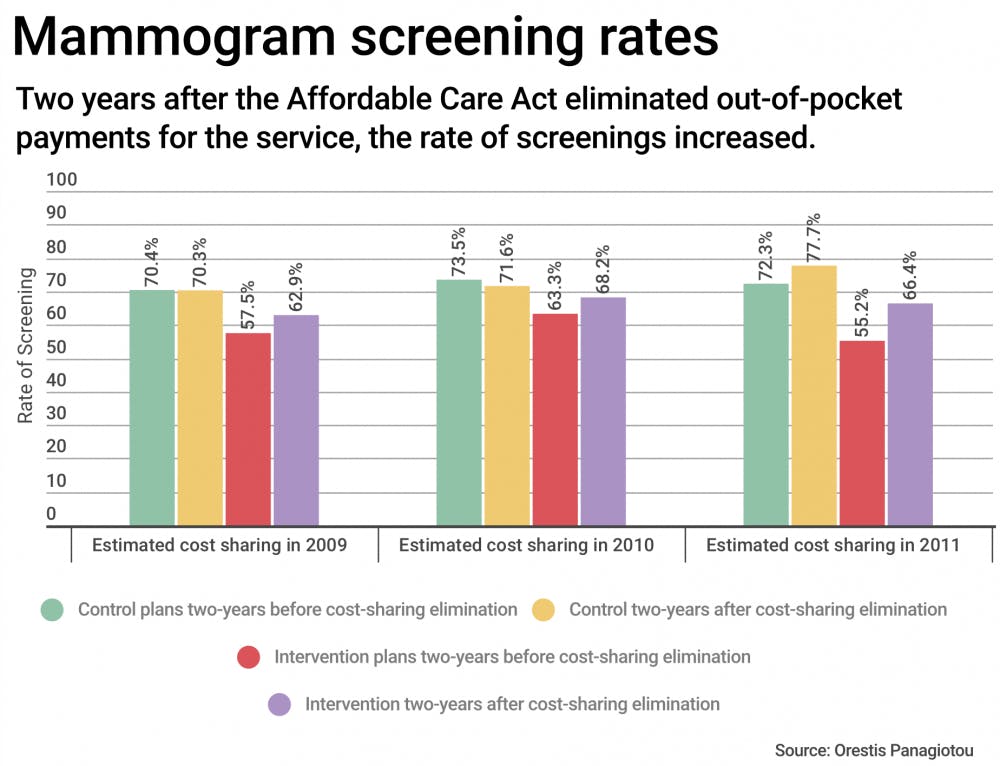
A study recently published in the New England Journal of Medicine found that mammogram screenings have increased in the two years after the Affordable Care Act eliminated cost sharing, or out-of-pocket payments. The study also examined the impact of this change on different demographics.
“The idea of eliminating copayments and making these services free is that more people would receive recommended services, but we had limited evidence as to whether that has actually happened,” said Amal Trivedi, lead author and associate professor of health services, policy and practice.
The study compared the number of mammogram screenings in the two years prior to the mandate to the number in the two years after it. Among people in Medicare Advantage Plans that eliminated copayments for mammograms, screening rates rose by about 6 percent, Trivedi said.
“Although (6 percent) may look like a small number, if you translate this to the number of women who are eligible to receive mammography, it is still a large number in terms of thousands more,” said Orestis Panagiotou, co-author and assistant professor of health services, policy and practice.
“The results show that the elimination of cost sharing as part of the ACA is an effective strategy for increasing use of recommended preventative services such as breast cancer screening,” said Bryan Leyva MD’18, co-author and a medical student.
“More women received recommended breast cancer screening after the ACA eliminated copayments,” Trivedi said. “This is good for public health because we have compelling evidence that receiving recommended screenings reduces mortality from breast cancer.”
The study also compared the changes in number of mammogram screenings among different demographics. “We found that women who lived in areas with lower education and also Hispanic women did not increase their use of screening mammography as much as women did in areas with higher education and white women. This suggests that there is a need to have more outreach to women with lower socioeconomic status, as well as Hispanic women, to make sure that they are aware of the important provisions of the Affordable Care Act and can benefit from these services to the same degree as other women,” Trivedi said.
As for the implications of this research, Panagiotou said that while it is still too early to say what concrete impacts there will be, follow-up data will help track how health care policies alter mammogram screening rates going forward. These policies may one day be transferable to increase the usage of other beneficial services, Panagiotou said.
Leyva also brought up the impact of future policy on the results that have been observed. “Any policy that attempts to get rid of these provisions of the ACA may result in less use of this recommended service,” he said.
Although there has been an increase in screening rates, Trivedi said that they remain suboptimal. “There are other costs associated with a screening that can be substantial and can be a barrier to receiving screening,” Trivedi said. These costs could include having access to a source of care, as well as the out-of-pocket costs that would arise if a screening produces false positives and demands further tests.
“Patients shouldn’t have to pay for things that are proven to be beneficial,” which is why it’s important to look into these kinds of policies and examine their outcomes in retrospect, Panagiotou said.
“In my opinion, it is a tragedy that there are women dying from late-stage breast cancers that could be prevented with appropriate screening and follow-up care,” Leyva said. “Policies have an important role to play in promoting or deterring use of recommended tests.”