A new University study published in Molecular Cell examined the specific amino acid changes that cause damaging processes associated with ALS and the dementia that results from it.
Amyotrophic lateral sclerosis, more commonly known as ALS, is a disease involving the death of neurons that control voluntary muscles. As these neurons die, patients lose the ability to control these muscles, and eventually lose the abilities to speak, eat, move and even breathe. The research studies the disease at a molecular level, following the way changes in amino acid sequences can affect the behavior of the family of proteins linked to the disease.
There are two types of ALS: Sporadic ALS, which accounts for about 90 to 95 percent of ALS cases, can affect anyone and any area of the body, while familial ALS, accounting for 5 to 10 percent of ALS cases, refers to inherited cases of the disease.
Right now, no effective treatments exist for either form of the disease, but the best upcoming treatments focus on familial ALS. “For the rest of the patients, we’re trying to understand how to change the protein directly,” said Nicolas Fawzi, assistant professor of medical science and co-author of the study.
Many of the proteins associated with the disease contain “low-complexity regions,” which, unlike parts of proteins that we traditionally study, are disordered and lack definite structure. These proteins are flexible, constantly changing shape. Fawzi explained that while scientists do not have a clear understanding of these proteins, due to the lack of clear, structural images, they know them to be functionally important.
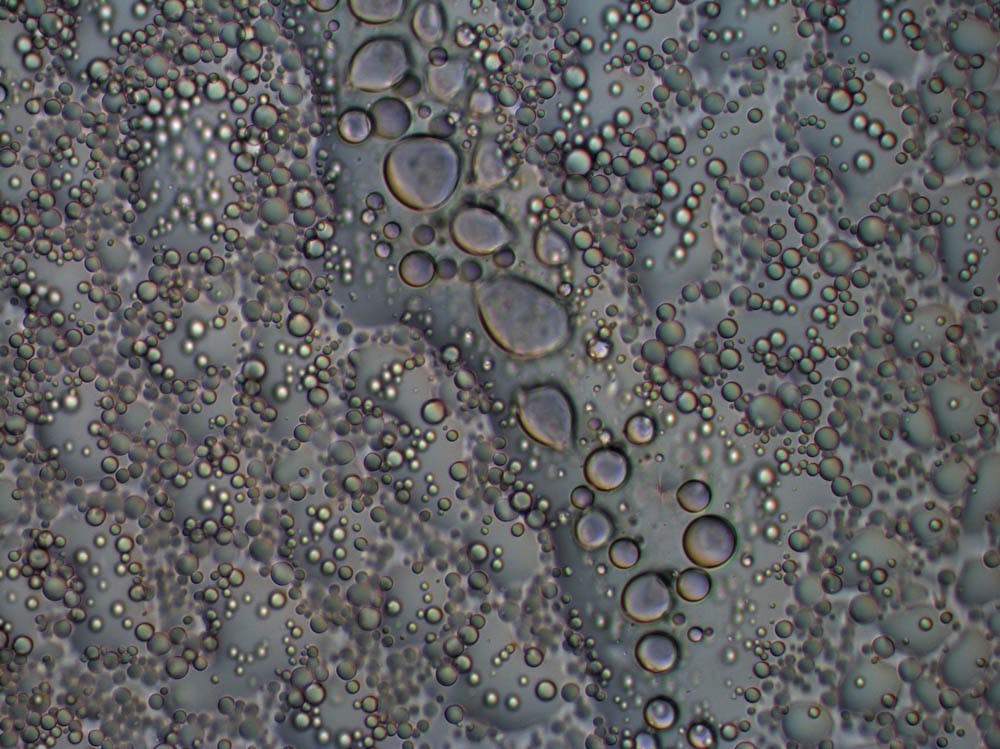
Some of these proteins undergo phase transition, forming droplets in the cells similar to those we see when oils are mixed with water, Wayne Bowen, professor of pharmacology, explained. These droplets, known as membrane-less organelles, are where the functions of these proteins, such as RNA processing, occur.
“When these interactions go awry, the proteins transition out of the droplet phase and form solid clumps,” Bowen said. “These proteins aggregates have been found to be toxic to the cells. Depending on the type of cell, this process may cause cell death.”
Fawzi’s study focuses on one of the proteins that is mutated during disease. Using computer simulations and analysis based on radio waves, the study demonstrated how small changes in the amino acid sequence of this protein could result in an increased propensity for the proteins to aggregate and form solid clumps that may damage the cells.
The computer simulation component of the study was led by Jeetain Mittal, associate professor of chemical and biomolecular engineering at Lehigh University.
Mittal and his team have been comparing the data produced by his models to the data obtained from the experiments, trying “to see if these models can be trusted to the point where they can be used confidently,” he said. “Computer modeling can allow us to represent the dynamic structure of the proteins and can, when accurately represented, give us a more detailed view of the structures,” Mittal said.
Using similar techniques, studies have also demonstrated that particle-level processes could alter the propensity of proteins to form droplets.
“By studying these different interactions, we can attempt to understand the underlying causes of the disease, and ultimately, if we can understand the cause, we can develop a drug or process that can prevent aggregation,” Bowen said.
“While this research doesn’t directly lead to treatment, we are hoping that our insights can tell us how the proteins behave, and what we can do to change this behavior. This can be useful for testing ideas and treatments in the future,” Fawzi said.