Researchers at the School of Public Health compared data from 2011 through 2014 to determine the effects of the Affordable Care Act on the number of people covered by health insurance and the quality of care at federally funded community health centers for a study published in the healthcare journal Health Affairs January.
According to the study led by Megan Cole GS, a PhD candidate in the School of Public Health, many adults gained access to health insurance under the ACA in 2014 when 25 states and Washington, D.C. expanded Medicaid eligibility for low-income and non-elderly individuals. Prior to the ACA, most states did not cover childless adults, Cole said. With the expansion of Medicaid, this population gained coverage along with “persons with incomes up to 138 percent of the federal poverty level,” she added.
The goals of extending Medicaid coverage were to “improve access to care for low-income patients who otherwise would not have access to health services and to protect people from large out-of-pocket expenses for healthcare,” Amal Trivedi, associate professor of health services, policy and practice, said.
Before analyzing the data from federally funded community health centers, the researchers developed three main hypotheses. The first hypothesis was that expanded eligibility would increase the proportion of patients with insurance. This hypothesis was based on data in nine states that showed fewer patients who visited health centers after the Medicaid expansion were uninsured. The second hypothesis was that health centers in expansion states would “see an increase in the number of unique patients served, compared to centers in non-expansion states.” Their third hypothesis was that gains in coverage “would translate into improved access to effective primary care, specialty care and prescription drugs for newly insured patients,” which would ultimately improve the quality of care.
After comparing data from health centers in expansion and non-expansion states, the researchers found their hypotheses held true. “In the states that expanded Medicaid under the (ACA), we observed very large increases in proportion of health center patients with Medicaid coverage and corresponding decreases in the fraction who are uninsured,” Trivedi said. The researchers also found “there was an increase in quality of care in health centers in the Medicaid expansion states,” Trivedi added. “There are a couple reasons for this, one of which might be due to increased insurance revenues to the community health centers.”
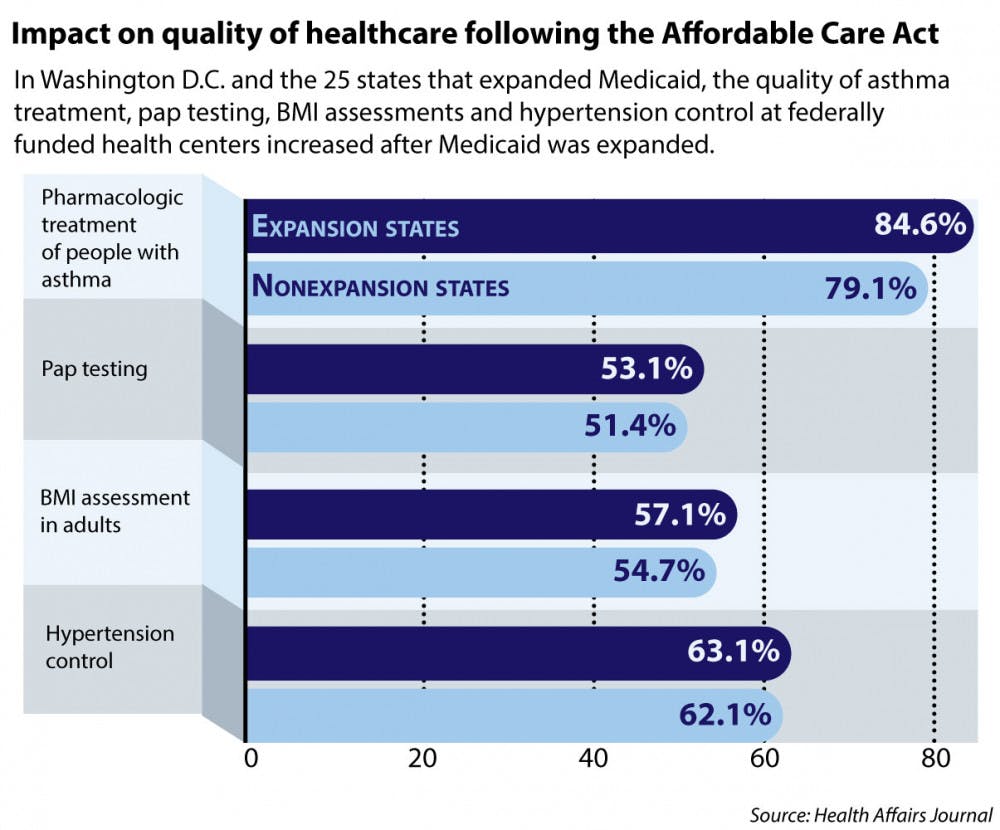
The researchers chose eight measures, such as colorectal cancer screening and diabetes control, to determine the quality of care at the health centers based on recommendations for improvement by the Centers of Disease Control and Prevention, said Omar Galárraga, assistant professor of health services, policy and practice and co-author of the study. Medicaid expansion ultimately was associated with improved accessibility on four of the eight measures examined: asthma treatment, Pap testing, body mass index assessment and hypertension control.
The results of the study show that repealing the ACA could result in those currently insured to “lose access to care, which could potentially reverse some of the positive effects that we observed in the first year,” Cole said. Yet it is unclear how expansion of Medicaid under the ACA will be affected by the new presidential administration, Galárraga said.
“The new administration has vowed to repeal the ACA. However, they still have not come out with a plan of what they are going to do,” Galárraga said. “If they repeal the law, millions of people will be affected — this is very unfortunate.”