New research conducted by Associate Professor of Medicine and Health Services, Policy and Practice Amal Trivedi indicates that reduced drug costs for indigenous people in Australia are associated with a significant decrease in the rate of hospitalizations for chronic conditions. The study, published in the Journal of General Internal Medicine this fall, was conducted as part of Trivedi’s Australian-American Health Policy Fellowship. Four other Australia-based researchers collaborated on the research.
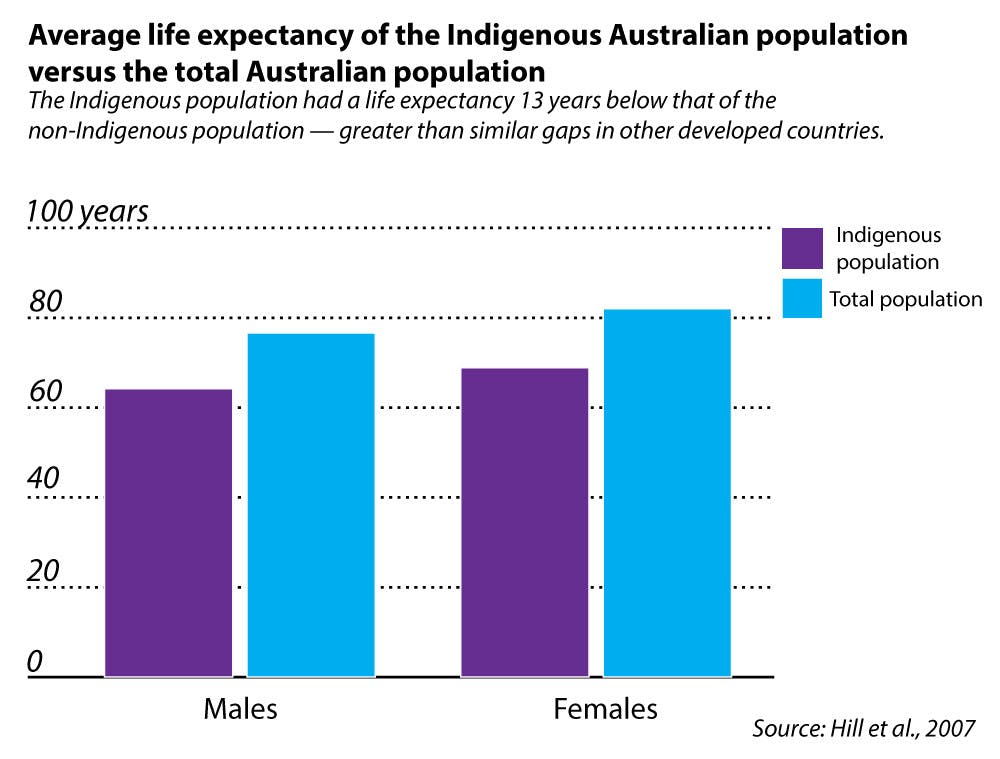
Trivedi said his motivation for the study arose from a “long-standing interest in health disparities and in policies and policy strategies to address disparities in … health outcomes.” The study investigated the Closing the Gap Pharmaceutical Benefit Scheme, a policy intended to reduce the 13-year difference in average lifespan between indigenous and non-indigenous people in Australia. Implemented in July 2010, PBS reduced drug co-pays for indigenous peoples from $33.30 per prescription to $5.40, while those already receiving subsidized co-pays of $5.40 now received the drugs for no co-pay.
Margaret Kelaher, co-author and director of the Centre for Health Policy at the University of Melbourne, said the drastic lifespan difference could be attributed to the legacy of colonization. “The fact that people were taking the land … contributed a lot to much poorer outcomes — in education, in income and in a range of factors that contribute to health,” Kelaher said. One of the reasons the government decided to lower drug costs was because the disparity between aboriginal and non-aboriginal Australians is largely due to poor management of chronic disease, she added.
Upon studying the PBS initiative in 24 different sites in Australia, the researchers compared the regions with the greatest and lowest uptake of the incentive. “We found that there were greater reductions in hospitalizations in areas where there was higher uptake of the incentive,” Trivedi said.
But this finding did not extend to non-indigenous populations nor acute hospitalizations. Researchers believe this may be because acute hospitalizations usually address conditions for which better drug adherence does not significantly impact the rate of hospitalizations, such as urinary tract infections and pneumonia.
“The potential mechanism is that out-of-pocket costs are a barrier to using effective drug therapy to treat common chronic conditions like diabetes or heart disease,” Trivedi said. He said he saw the same trend in his clinical practice: When patients are not able to adhere to their chronic medications, their conditions can worsen, leading to a hospitalization. These hospitalizations are risky and disruptive for patients, as well as expensive to the healthcare system, he added.
Measures similar to the PBS initiative are already in place in the United States under the Affordable Care Act. “There are cost-sharing subsidies to reduce co-payments for Native Americans who are enrolled in insurance exchanges,” Trivedi said. “We still don’t have evidence of the impact of those cost-sharing subsidies, but at least our work in Australia found enough association between reducing out-of-pocket costs for vulnerable, low-income, ethnic minority populations and lower rates of being hospitalized for chronic conditions.”
Vincent Mor, professor of health services, policy and practice, linked the study’s results to other findings in the field. “We had a paper on the Medicare Advantage plan, where we looked at plans to increase the co-pay for primary care visits,” he said. “Those visits declined, and hospitalizations increased … particularly for minorities and people who live in poor areas.”
“The next step in this research is … to use more granular data — data at the level of patients — to compare outcomes for those who did and did not register for the incentive,” Trivedi said.
Mor also said researchers should further investigate the effect of reduced co-pays in the context of similar socioeconomic dynamics in the United States. Likewise, Kelaher said “this research … provides an evidence base for broader initiatives that might target other disadvantaged populations.”
Trivedi and his Australian colleagues report plans for continued collaboration in the future. Trivedi said the collaboration is a valuable exchange of mutual learning between the two countries. “One of the main objectives of the fellowship … was to see what we can learn from the Australian healthcare system and what lessons from American healthcare policy will be applicable to Australian healthcare,” he said.