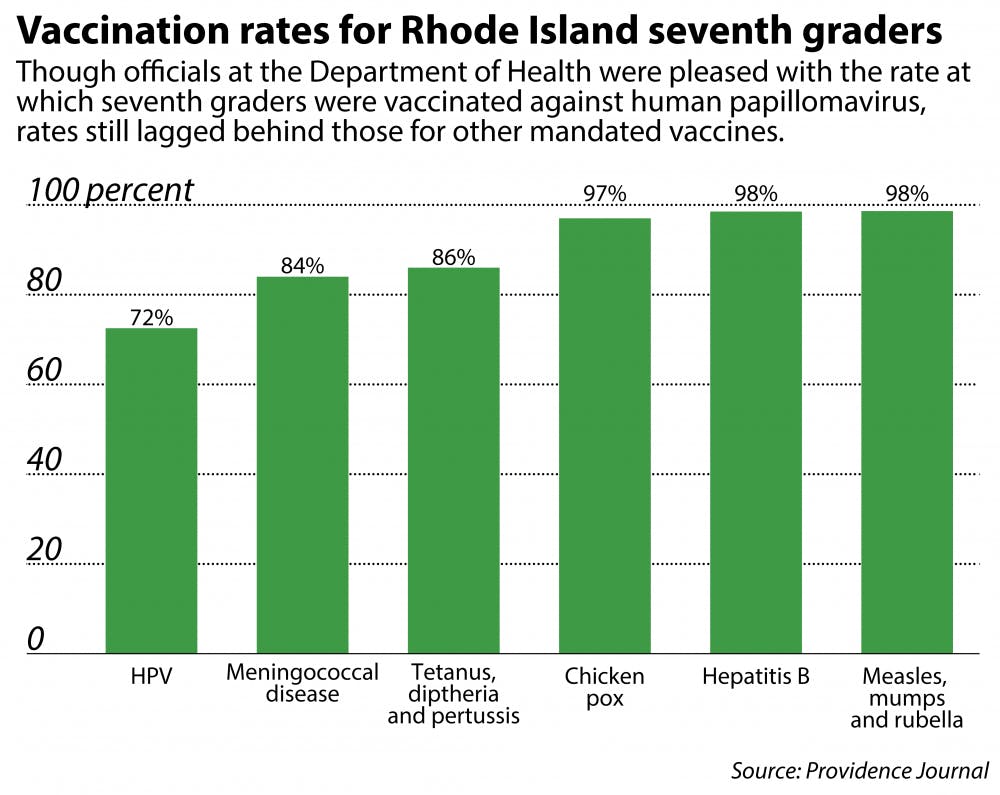
After mandating a first dose of the human papillomavirus vaccine for all students entering the seventh grade, the Rhode Island Department of Health estimates that almost three-quarters of seventh graders had received their first dose by the first day of the 2015-16 school year, said Joseph Wendelken, acting public information officer for RIDOH.
The actual percentage might be even greater in the Ocean State, which already boasts one of the highest HPV immunization rates in the country, Wendelken said. The percentage does not take into account students who had vaccinations even a week after the first day of school due to extenuating circumstances such as delayed physical examinations, he added.
RIDOH passed the mandate in July 2014, and it officially took effect Aug. 1, The Herald previously reported.
“We expect that number to keep climbing,” Wendelken said. “It’s typical that when a vaccine is incorporated into the school immunization schedule, it starts at a baseline and starts to creep up as doctors, parents and school administrators get used to that being a part of the routine.”
Some Rhode Islanders have expressed reluctance to accept the decision, both because of the nature of the mandate and because of the association of a sexually transmitted disease with young children.
Aimee Gardiner, director of outreach for Rhode Islanders Against Mandated HPV Vaccines — a nonprofit created to oppose the mandate — said the organization and others favor “standing for our rights and for not having an overreach of government.”
“The problem is not about the vaccination itself whatsoever,” Gardiner said. Rather, the organization takes issue with the government mandating a vaccination for a disease when it does not impact a child’s education.
Gardiner said that the organization has three main goals with regards to HPV vaccinations: to make HPV vaccinations an option instead of a mandate, to make it more difficult for RIDOH to mandate another vaccination in the future and to advocate for informed consent. Once a vaccine is mandated, “all the risks and benefits that the patient has the right to know tend to go by the wayside,” she said.
Gardiner said she believes the decision of whether or not to vaccinate should rest solely with families. If an HPV vaccination is antithetical to its beliefs, a family can declare a religious exemption by completing a RIDOH form, she said.
Wendelken said he believes it is important that children are vaccinated around the seventh grade because the vaccine is most effective when administered to 11- and 12-year-olds. He stressed the fact that though HPV is transmitted sexually, children have the greatest response to the vaccine if it is administered “long before there’s any sexual contact.”
“The HPV vaccine protects against a virus that we know leads to cancer, and it’s incredibly beneficial and valuable,” Wendelken said. “Now it’s up to doctors across the country and state to try to communicate to parents the importance of this immunization.”