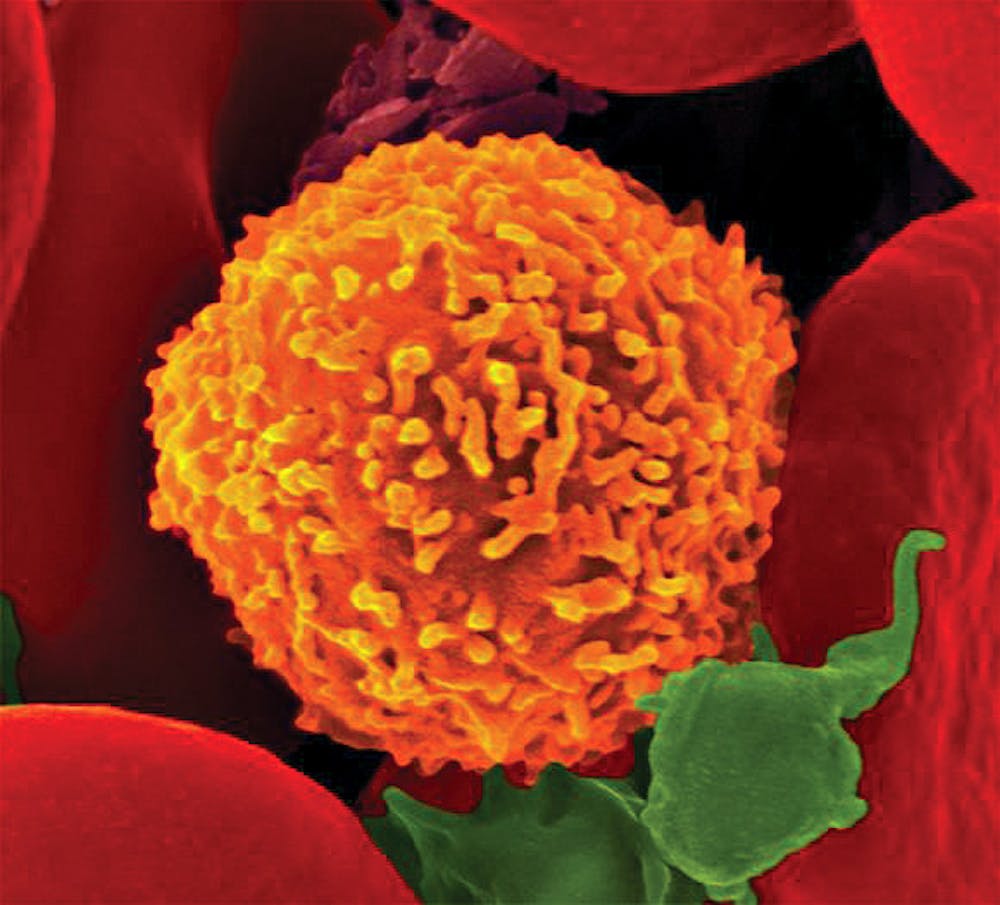
The immune system may be more versatile than scientists once thought, according to a new study by Brown researchers.
Scientists usually separate the immune system into two branches. Innate immunity rapidly targets a wide variety of pathogens by unleashing natural killer cells and innate cytokines — proteins that act as signals between cells. These reactions trigger adaptive immunity, which is a pathogen-specific response. Adaptive immunity has a slower onset the first time the immune system encounters a new pathogen, but in future instances can respond rapidly, recognizing the pathogen from previous exposures.
But according to the new study, certain cells associated with adaptive immunity — CD8 T-cells — can also behave like natural killer cells. The research was published in the journal mBio earlier this month.
Scientists know that many other types of T-cells can transition between innate and adaptive immunity, said Manish Butte, an assistant professor of pediatrics at Stanford University who has done extensive work in immunology but was not involved in the study. “We’ve known this for well over a decade, but what’s new is that CD8 T cells can do that, too.”
In a previous study, other researchers had seen that CD8 T-cells produce more of the protein STAT4 after encountering an infection. This makes them more like natural killer cells, which have high STAT4 and thus are more sensitive to innate cytokines, proteins that act as signals between cells, said Christine Biron, lead author of the study and professor of medical science and molecular microbiology and immunology.
“We wanted to know: Do CD8 T cells maintain that characteristic when they become memory CD8 T-cells?” Biron said.
In their research, scientists exposed mice to a strain of a virus and then extracted their T-cells to examine how they interacted with various cytokines. While not all the T-cells adapted to the virus, the ones that had were much more sensitive to cytokines.
To determine whether it was STAT4 that increased the T-cell’s responsiveness, scientists examined mice that were genetically engineered to cease production of STAT4 proteins. They then exposed the mice to the virus twice, and saw that while both mice did increase CD8 T-cell levels after an initial infection, only the mice with STAT4 were able to produce an innate response when they were exposed to the virus for a second time.
In another experiment, scientists tested how mice with and without exposure to the first virus would react when exposed to a new virus. The mice who had been exposed to the first virus showed a faster immune response to the novel pathogen, which included an increase in cytokine production by the memory CD8 T-cells.
“This shows the immune system is very flexible in responding to different infections,” said co-author Margarite Tarrio GS, who studies pathobiology.
“The immune system is using a limited number of genes to fight a possibly infinite number of different microbes,” Biron said.
The results of the study may “help with vaccine protocols to give the best defense,” she added. Vaccines trigger the body to produce antibodies, which may help prevent and slow down an infection and can be optimized to induce the body to create a large amount of antibodies.
“If this innate-like response of CD8 T-cells is functionally important for an effective and rapid immune response, then perhaps vaccines should be developed that promote the development of memory CD8 T-cells capable of functioning in an innate-like manner,” wrote Yoji Shimizu, the director of the Medical Scientist Training Program at the University of Minnesota at Twin Cities, in an email to The Herald.
“The identification of STAT4 as an important protein involved in this response is also significant, as this finding provides an intracellular target and marker that we can use to identify these cells and maybe manipulate the function of other memory T-cells,” Shimizu wrote. He added that he is interested in figuring out whether human CD8 T-cells behave the same way the mouse CD8 T cells that the researchers studied.
“We also know now that there are lots of different types of memory CD8 T-cells, and it will be fascinating to see what specific types of memory CD8 T-cells have this innate-like property,” Shimizu wrote.
“Our study suggests that vaccines, in general, can help lead to a pool of cells that might actually be helpful to fight off completely different viruses and new antigens,” Tarrio said.
Biron said she plans to study vaccinations and determine their effect on the balance of CD8 T- and natural killercells. “We have to more finely define innate immunity versus specific immunity,” she added.
ADVERTISEMENT